

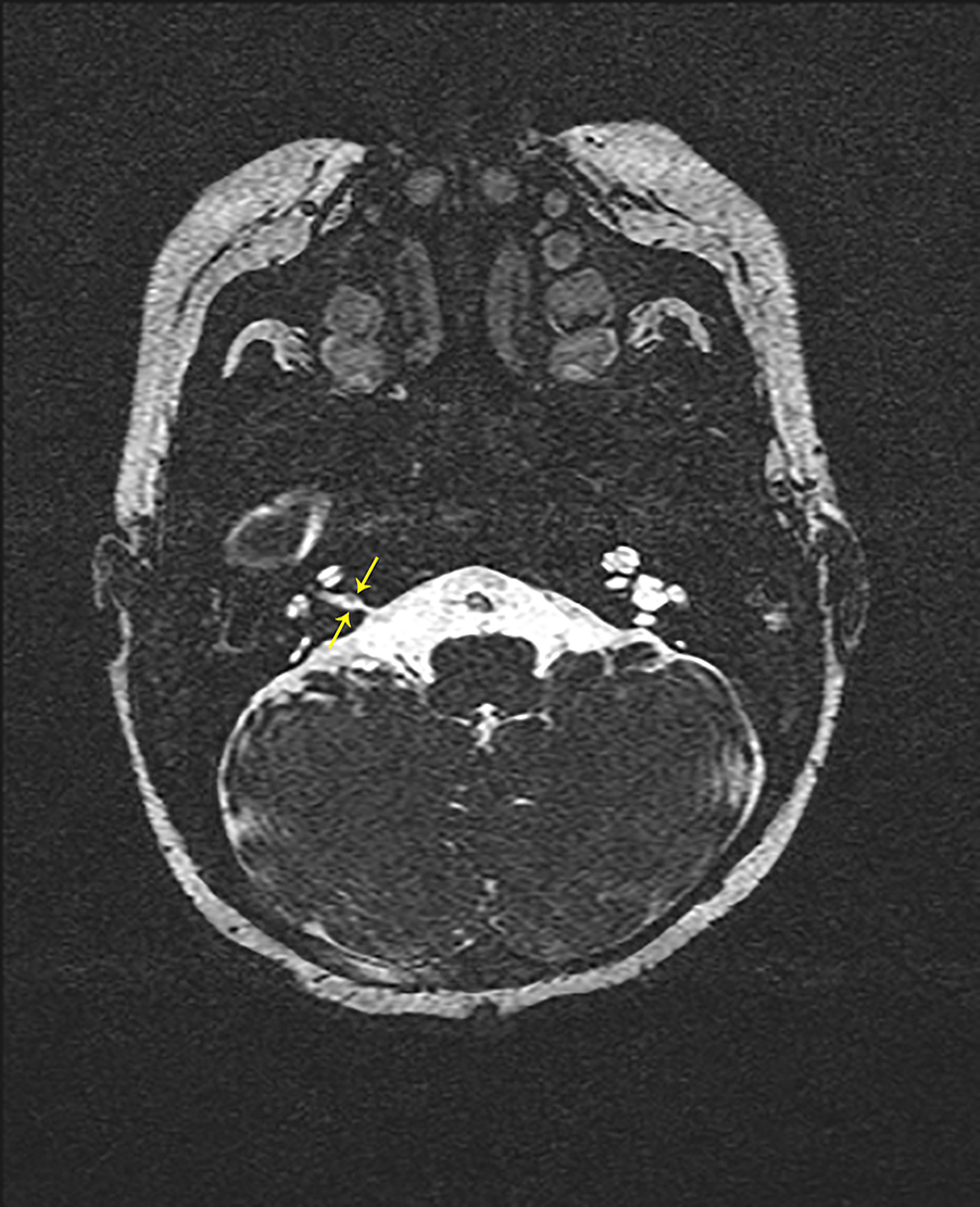
This increase in size tends to occur early, and follow-up CT in 3 months and 6 months would be appropriate in further evaluation. In oncologic patients, 28% of small pulmonary nodules detected at initial CT will increase in size, suggesting metastasis. Combined, 28% of patient' s nodules increased (90% were within 365 days 25% within 203 days and 14% within 14 days). For those with greater than 365 days follow-up, the observed nodule was increased (3, 5%) stable (51, 93%) and stable but new nodule developed (1). For those with less than 365 days, the observed nodule was increased (17, 36%), increased and new nodules (9, 19%) stable (19, 40%) stable but new nodules developed (1) and decreased (1). There were 102 cases that met criteria for inclusion.įorty-seven had follow-up CT of less than 365 days, and 55 had follow-up CT for more than 365 days. All CT images were evaluated by two thoracic radiologists for nodules 4 mm or less. This tumor extends from the internal auditory canal into the intracranial space, compressing brain tissue but not. Based on this finding, a presumptive diagnosis of neurofibromatosis Type II was made, which was initially managed conservatively with close observation. Initial magnetic resonance imaging revealed bilateral nonenhancing IAC/CPA tumors. Radiology reports of thoracic CTs from a 2-year period were searched for keywords indicating a small pulmonary nodule. Description: We report a case of a 58-year-old male who presented with hearing loss, tinnitus, and vertigo. We evaluated a group of oncology patients to determine the outcome of small pulmonary nodules and whether they can be ignored in the therapeutic decision process. It remains unclear whether a non-surgical therapy such as radiation therapy is an alternative treatment option for growing choristomas.It is often not possible to determine whether small nodules detected on computed tomography (CT) in oncology patients are metastatic. Due to a lack of access for biopsy, lesions in the IAM are often only diagnosed after surgical removal. Therefore, choristomas are usually misdiagnosed as the more common VS initially. However, choristomas cannot be distinguished from other tumors in the IAM such as VS. Osteomas are hypointense in all sequences and non-enhancing after contrast. Lipomas can usually be recognized by their hyperintense signal in T 1-weighted MRI and can be confirmed by fat suppression techniques. Vascular tumors like hemangiomas tend to be more hyperintense in MRI. Meningiomas can be distinguished from other tumors by the presence of calcification, dural tail and bone infiltration. Schwannomas of the facial nerve may extend into the labyrinthine facial nerve canal, and this feature could distinguish them from other tumors. The latter are less common in MRI at this location and include astrocytomas, ependymomas, papillomas, hemangioblastomas and metastases. Tumors in the IAM can be classified into 2 groups depending on their location: there are extra-axial lesions (outside the brain parenchyma) such as VS, meningiomas, epidermoid cysts and paragangliomas, and rare tumors such as schwannomas of the 5th, 6th, 7th, 9th, 10th, 11th or 12th cranial nerve, and vascular lesions and there are intra-axial lesions (within the brain parenchyma). How can choristomas be differentiated from other tumors in the IAM? Contrast-enhanced MRI may be helpful. Two of the patients with hearing loss presented additionally with tinnitus, 1 patient reported additionally the loss of balance and another patient tinnitus and the loss of balance. All patients suffered from a hearing loss with the exception of 1 patient with hyperacusis and 2 additional patients in whom the hearing status was not reported. In 4 of 11 cases published in a complete clinical review, the tumors contained also skeletal muscle cells which were not found in our case. All contained smooth muscle cells as a major component, connective tissue and nerve fibers. The reports did not say whether the choristomas were removed due to growth or due to the symptoms they caused. We found only 14 reports of cases of choristomas of the 8th cranial nerve, which were all removed surgically. Smooth muscle tissue does not represent a component of cranial nerves and we suggest that the correct classification for this lesion is neuromuscular choristoma and not hamartoma. The tumor in our report consisted of smooth muscle tissue, nerve fibers and adipose tissue. Neuromuscular choristomas in the IAM are exceedingly rare lesions.


 0 kommentar(er)
0 kommentar(er)
